Sleep apnea could potentially be a serious sleep disorder. There are several different sleep apneas and they cause difficulty breathing while sleeping. Some of the symptoms include loud snoring, episodes of stopped breathing during sleep, awakening with a sore and dry throat, morning headache, high blood pressure, mood disturbances, and more. Thankfully, there are several treatment options for it. Some people only experience it while lying on their back so it’s recommended to sleep on your side. People with existing nasal problems need to tend to those first by using sprays and similar. In some cases, even sleeping pills help. There are even mechanical devices that help with sleep apnea. The most famous one would be the CPAP machine. This machine helps clear your airways by wearing a mask that contains a gentle air blower which forces air through the nose and mouth. If none of this helps, you can opt for a surgical procedure like a tonsillectomy or nasal surgery.
Would you like to know more? Read below the article by Dr. Samir Lahzami.
SLEEP APNEA: WHEN SLEEP MAKES YOU SICK
Do you snore, wake up with a headache and a feeling of unresponsive sleep, feel a lack of energy & concentration, and struggle not to fall asleep during the day? You are definitely suffering from sleep apnea syndrome (SAS)!
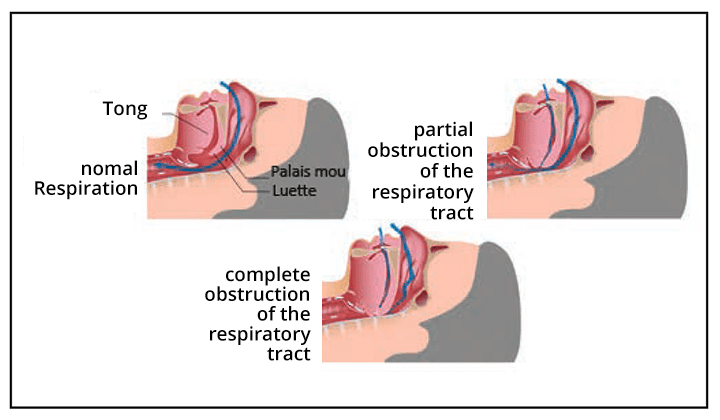
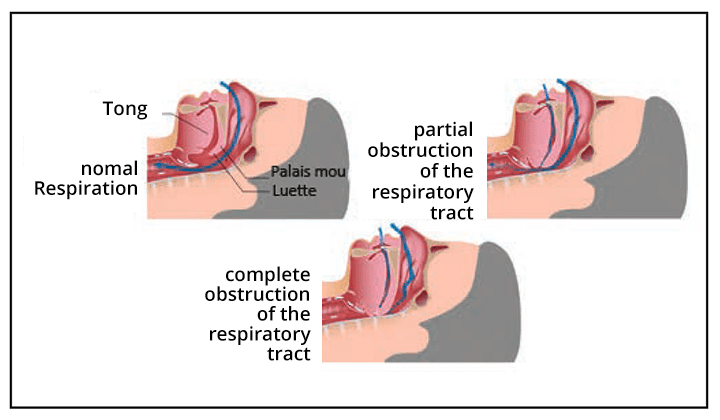
SAS is defined by the presence of apnea (stopping breathing for at least 10 seconds) or hypopneas (decrease in respiratory flow associated with a drop in blood oxygen level) during sleep, associated with daytime sleepiness. The vast majority of SAS is of obstructive origin, that is to say, linked to an obstruction partial or total of the throat. In fact, the muscles relax physiologically during sleep and reduce the opening of the back of the throat. Fortunately, this did no effect on the breathing of the majority of people but can be the cause of snoring and apnea/hypopnea when the reduction is more significant or complete (Figure 1). In these cases, an increase in respiratory effort in an attempt to maintain sufficient airflow follows, which leads to micro-alarms necessary to reactivate the tension of the muscles of the back of the throat, with consequently a disturbing quality of sleep. SAS of central origin, related to respiratory control dysfunction automatic during sleep, is much rarer and associated with cardiac or neurological pathologies. It is not the subject of this article. SAS affects 3 to 7% of the general population, with a male predominance. The prevalence increases with age and reaches 10 to 20% in those over 65. Being overweight is the main predisposing factor, but people with normal weight may also suffer from it due to anatomical factors congenital (broad tongue base, indented mandible, etc.). Consuming alcohol, opiates, or sleeping pills increases the risk or severity.
WHAT ARE THE SYMPTOMS?
The vast majority of patients with SAS snore, but fortunately the opposite most often does not hold true. Many other manifestations during sleep may occur: restless sleep, waking up suddenly with a feeling of suffocation, difficulty breathing at night, night sweats, frequent waking up to urinate, bedwetting, somnambulism, and hypersalivation. Sometimes the patient does not perceive any of these symptoms, in which case the partner may fortunately often notice loud snoring interspersed with breathing pauses.
Daytime consequences of SAS-related sleep disturbances are dominated drowsiness, responsible for a decline in the quality of social and professional life, as well as an increase in the risk of traffic accidents. This sleep poor quality can also be manifested by morning headaches, memory and concentration problems (within particular worsening of cognitive disorders in the elderly), lack of energy, behavioral disturbances, irritability, depressive syndrome, and libido disturbances. These symptoms are often wrongly blamed on aging or overwork.
WHAT ARE THE CONSEQUENCES FOR HEALTH?
In addition to the manifestations mentioned above, untreated SAS has harmful consequences from a cardiovascular point of view. It increases the risk of high blood pressure and may be responsible for poor control of pre-existing hypertension. The risk of cardiac arrhythmias (especially atrial fibrillation) is also increased, same as the occurrence of myocardial infarction, heart failure, and accidents cerebrovascular.
According to recent studies, people with SAS have an accumulation of abnormal beta-amyloid protein in their brains. This is the main component of amyloid plaques involved in Alzheimer’s disease. SAS could therefore long-term promote the occurrence of certain neurodegenerative conditions.
HOW TO CONFIRM DIAGNOSIS?


SAS should be suggested and looked for in the presence of symptoms suggestive, poorly controlled high blood pressure, or overt cardio or cerebrovascular disease. As the symptoms are sometimes absent or perceived as normal by the patient, several predictive scores for SAS have been developed. The “NoSAS score” is one of them and can be used in self-test via an application for smartphones. Like everyone else predictive scores of SAS, it has high sensitivity but relatively low specificity. It, therefore, makes it possible, in the event of a negative result, to reasonably exclude the presence of a SAS, but its positivity does not confirm its presence.
Confirmation of the diagnosis requires nighttime polygraphy to be performed by a pulmonologist. This is a home exam which combines nasal air flow sensors, oxygen saturation, and heart rate, a fabric abdominal and chest strap (for analyze respiratory movements), as well as a position sensor (figure 2). A night’s sleep laboratory (polysomnography) is sometimes necessary to clarify the diagnosis.
The result of nocturnal polygraphy is expressed in a number of apneas-hypopneas per hour (index apnea-hypopnea, IAH). Although the criteria are debated, an SAS is recognized as significant from an IAH ≥ 15 / h and its degree is severe if the AHI is ≥ 30/h.
WHAT ARE THE THERAPEUTIC MEANS?
Treatment of SAS depends on its degree of severity, cardiovascular risk factors, and co-morbidities, as well as the extent of daytime sleepiness and other symptoms. The goal of treatment is to maintain the patency of the pathways air during sleep.
Simple measures, such as abstinence from alcohol and sleeping pills at night, can sometimes suffice in mild cases. In obese patients, obtaining a loss of weight is always recommended, it can reduce the severity or even make SAS disappear. In patients with apnea only in the supine position, there are specific devices to wear at night that prevent sleeping on the back.
For cases of mild to moderate SAS, a mandibular advancement prosthesis may be proposed. These are gutters molded on the teeth that will provide traction on the lower jaw to increase the opening of the throat. However, these devices are only really effective in certain patients and allow, where if necessary, a halving of the number of apneas/hypopneas on average. Furthermore, negative effects on the temporomandibular joints may develop in the long-term use case.
Surgical options, once widely practiced, are now only recommended in very rare cases, especially in cases of significant hypertrophy of the tonsils.
The treatment of choice for SAS is CPAP (“Continuous Positive Airway Pressure”), a device that allows you to breathe air in the airways with continuous positive pressure, and so prevent collapse. The patient is connected to the device by a mask whose choice is crucial. There are many models, which can be based on nostrils, cover the nose alone or the mouth and the nose at the same time (figure 3). Once difficult to tolerate, these devices are now quiet and patients usually get used to them well. When used regularly and properly adjusted, CPAP provides complete correction of SAS.


CONCLUSIONS
SAS is a common pathology often responsible for nocturnal symptoms bothersome and disturbed sleep quality leading to drowsiness diurnal. It significantly increases the risk of developing cardiovascular disease. It is also probably a risk factor for certain conditions neurodegenerative. If SAS is suspected, nocturnal polygraphy should be performed to confirm the diagnosis. Depending on its degree of severity and its characteristics, several treatments may be recommended, but CPAP is the most effective treatment.











0 Comments