For the first time in 1743, the famous surgeon of Louis XVI, François de La Peyronie, described this condition, which is usually a hardening of the corpus cavernosum accompanied by pain and curvature of the penis during erection. Unlike other male sexual pathologies, where patients are reluctant to see a doctor, patients turn to a specialist relatively quickly for this limiting pathology, which usually begins with a painful fibrous nodule.
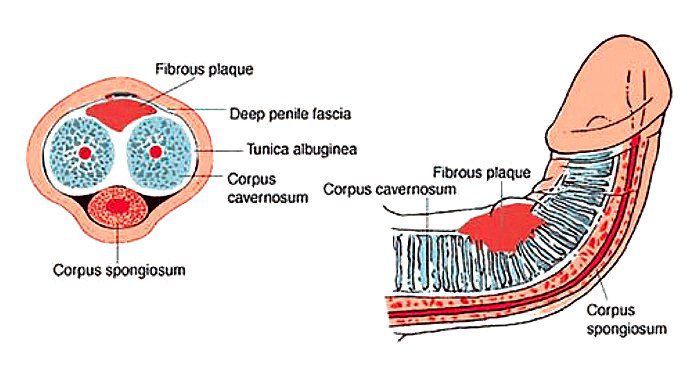
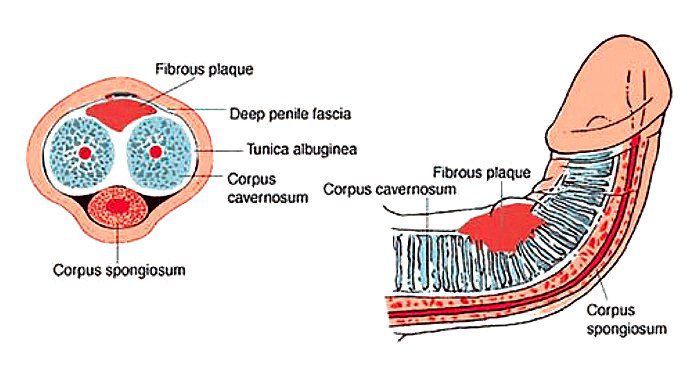
The incidence of the disease is highest between the ages of 50 and 65, but it can also occur at a young age and sometimes even in adolescence, especially in the congenital form. This pathology, which affects about 8% of the male population and whose exact cause is unknown, appears to be multifactorial in origin. Several theories have been proposed, including one that implicates microvascular trauma in the tunica albuginea during sexual intercourse. Indeed, it appears that in some genetically predisposed individuals, there is an alteration in repair processes that results in excessive production of TGF-ß1 (cytokine that results in the formation and maintenance of fibrosis of the corpus cavernosum.) Therefore, it would be an altered inflammatory response to trauma or repetitive strain injury in genetically predisposed individuals….
Patient procedure
In the initial phase, it is, of course, essential to reassure the patient through empathetic conversation and to confirm the diagnosis. During the anamnesis, possible previous traumas, even minor ones, due to “coitus faux pas” and sexual intercourse in extreme positions are sought. Metabolic disorders that may be associated with Peyronie’s disease include familial diabetes after age 50, hyperuricemia, hypertension, and atherosclerosis. After taking a history, the specialist performs a careful clinical examination by palpating and measuring the points of induration on the penis, not forgetting the septum. The rest of the examination also includes the search for possible prostatic, urological or even general anomalies. In fact, the fibrosis of the hand tendons known as Dupuytren’s contracture is sometimes associated with this urologic trophic disorder.
Further investigations
Ultrasound and Doppler ultrasound with or without injection of vasoactive substances (prostaglandin or papaverine) allow, above all, the assessment of plaque intensity and the extent of curvature with angular measurement, which subsequently provides guidance for treatment and, depending on the treatment chosen, allows follow-up and a prognostic factor. In rare cases, an MRI scan of the penis may be requested to look for tumor pathology (penile metastasis from prostate cancer, a rare but classic case) or hematologic disease, which usually causes priapism in addition to the curvature and inflammatory nodule.
• Medicinal and conservative treatments
For many years, treatments were limited to the prescription of vitamin E, known for its antioxidant properties, and certain drugs to relieve pain and inflammation. Some studies report therapeutic effects with interferon or intracavernosal or transdermal application of verapamil.
• Non-medication approaches
In extreme cases, such as the congenital form or when drug treatment proves insufficient, surgical treatment is considered. However, it must be mentioned that in all cases it is preferable to consider surgery between 9 months and two years after the onset of the disease, due to the progressive aspect of the pathology and the spontaneous regression of the plaques and fibrosis over time.
• Surgical techniques
Classically, plication of the corpus cavernosum using the NESBIT technique, with or without excision of fibrous tissue depending on the severity of fibrosis, has been and remains the surgical “gold standard” of pathology. Some of these plicatures are simple, non-invasive and do not alter erectile function in any way.
• Shock waves
Shock waves are mechanical waves, similar to acoustic waves, that can propagate through a medium. When these waves are applied to an organ or tissue, they release energy, causing compression and then expansion of the tissue encountered. The application of the low intensity mechanical wave to the endothelium of blood vessels results in the formation of biochemical signals that promote the formation of new small capillaries by growth factors. Principle of neo-angiogenesis. When the wave is applied to the corpus cavernosum, this phenomenon of neo-angiogenesis allows better permeability and increased blood flow to the corpus cavernosum, resulting in better penile function.
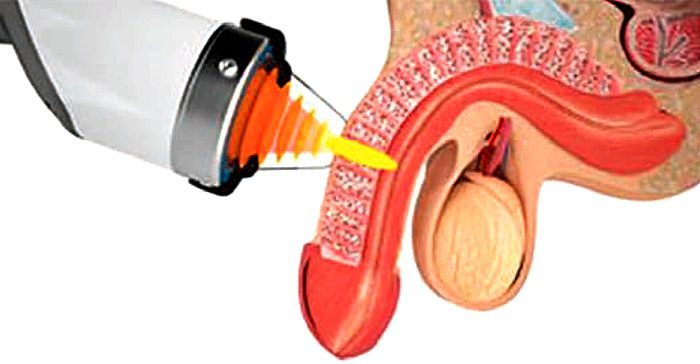
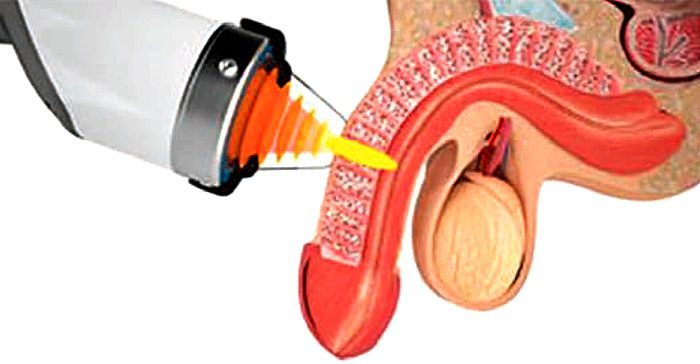
regeneration of the corpus cavernosum through the principle of neo-angiogenesis, thus improving penile function.
• IPP Combi
The IPP Combi is a device based on the principle of using low intensity mechanical waves applied to the penis. Although already known and developed for several years, the application of linear waves with the IPP Combi is an interesting and quite original approach. The technique is widely used in Europe and the USA and was introduced in Switzerland, where it is increasingly used, more than two years ago. The treatment is ambulatory and the recommended protocol is usually 6 applications, once or twice a week.
• Electroporation
This is a non-invasive technique, usually coupled with the application of mechanical waves, which consists in applying electrical current impulses to a surface such as the skin or a cell membrane. This procedure is used to open the pores or channels so that a substance can be introduced. In our treatment protocol we use an expertly prepared water-soluble 5 ml solution consisting of a mixture of hydrocortisone, verapamil and vitamin E.
In practice
The treatment is simple and is performed with a patient either lying down or in a gynecological position that allows better access to the external genitalia. The application of the waves lasts 10 minutes at low intensity and medium frequency, which can be adjusted according to the sensitivity of the patient and the quality of the tissue. The probe is applied directly to the corpus cavernosum by starting the session at a distance from the nodule and, if possible, in the healthy tissue to avoid pain when applying the energy to the sensitive area to be treated. The combination of IPP and electroporation (including a 5- to 10-minute application of the solution depending on the case) significantly improves therapy and functional outcomes. Usually, after 3 to 4 sessions, patients notice better spontaneous erections and softening of the nodule, which leads to a reduction in the doses of drugs used for erection (PDE-5 inhibitors).
Conclusion
Peyronie’s disease is a long-established condition, but has long been stigmatized as a malformation, has been misunderstood, and has generated shame and embarrassment on the part of patients. Specialized and nonspecialized physicians have sometimes taken an approach of denial or trivialization due to a lack of understanding of the pathophysiology as well as the proven ineffectiveness of many of the proposed treatments. Here we present a new achievement, namely the use of linear shock waves, a promising and very interesting element in the therapeutic arsenal. This technique, especially when combined with the use of PDE-5 inhibitors and electroporation, should make it possible not only to treat and improve the fibrous nodule by increasing the elasticity of the affected tissue, but also to activate the circulation of the penile corpus cavernosum. This double action contributes to the improvement of erectile function and gives hope to many patients who are desperately looking for a solution to their problem.











0 Comments