FUNGAL ALLERGY: CAUSES AND FREQUENCY?
For a century, fungal spores have been considered a possible cause of respiratory allergies. From the great kingdom of fungi, about 100 species of fungi have been associated with allergic respiratory diseases. In principle, however, only two classes of fungi are relevant for respiratory allergies, namely the tubular fungi (ascomycetes) and the pillar fungi (basidiomycetes). The “fungi imperfecti”, which represent the vegetative stage of the tube fungi, are considered to be mainly responsible for a fungus-induced respiratory allergy. Recognised and study-proven allergy-inducing fungal species are: Alternaria alternata (tenuis), Cladosporium herbarum, Aspergillus and Penicillium species.
The amount of spores in the air can be high throughout the year and can exceed that of pollen many times over in summer. The spore content inside flats and houses usually reflects the spore content of the air from the surroundings. However, the concentration indoors is on average 2/3 lower than in the open air. The sensitisation rate to fungal antigens is not very high, with only 1-3% of people tested with Alternaria and Cladosporium extracts showing a positive skin test or having specific IgE antibodies to these fungal allergens in the blood in cross-sectional examinations. Fungal allergies are most common in people who work in and with nature (e.g. farmers, gardeners) or who work with fungi professionally (e.g. breeders).
WHAT ALLERGIC DISEASES CAN FUNGI TRIGGER?
The clinical symptoms of a fungal allergy are no different from those of a pollen or indoor allergy. Fungal spores can cause rhinitis and/or conjunctivitis. As the spores are usually less than 10 μm in diameter, they easily enter the lungs and can cause respiratory distress, coughing and asthma attacks. It has been shown that large amounts of fungal spores in the atmosphere are sufficient to trigger severe respiratory symptoms (asthma), especially in young people, whether they are allergic to fungi or not. Apart from the classic respiratory allergy, fungal exposure can also lead to hypersensitivity pneumonitis (exogenous allergic alveolitis, “pneumonia”). This is caused by a high spore load and can also develop in living spaces (e.g. decorative fountains, air humidifiers, air conditioning systems). However, this type of lung disease is usually acquired through occupational exposure (e.g. farmer’s lung, malt worker’s lung, cheese washer’s lung, mushroom grower’s lung, vintner’s lung, bird keeper’s lung).
Occasionally, people who dispose of or compost vegetable waste may also be affected. Fungi can be the cause of chronic sinusitis. This is especially the case if the sinuses are overgrown with polyps. Here, spores or mycelia usually find favourable conditions for growth in the sinuses. Aspergillus species are often detected, but various fungi can be behind the clinical picture of “allergic fungal sinusitis”. Symptoms include obstructed nasal breathing, lack of sense of smell, discoloured (brown, blackish) nasal secretions, discharge of gummy discharges and often chronic headaches. However, allergic fungal sinusitis hardly differs from banal nasal polyps or chronic sinusitis. However, there is usually a marked eosinophilia in the blood (>0.5 G/l), an elevated total IgE (>500 kU/l) and sensitisation to fungal antigens.


Another rare immunological lung disease caused by fungal antigens is allergic bronchopulmonary aspergillosis (ABPA). This lung disease is considered an analogue of allergic fungal sinusitis. Patients usually have chronic asthma, which is difficult to treat (“difficult-to-treat asthma”), cystic fibrosis, or bronchiectasis (found on lung CT). Although different fungi can cause this lung-specific disease, Aspergillus species are often identified in sputum. ABPA may be manifested by a (progressive) worsening of asthma, severe coughing attacks or the expulsion of thick, brownish to bloody mucus plugs. The blood usually shows eosinophilia (>0.5 G/l) and markedly elevated total IgE (>1000 kU/l). Sensitisation to fungal antigens is generally required for diagnosis.
GOOD TO KNOW: Brochure available on: www.bundespublikationen.admin.ch
Contact eczema to fungi is usually confined to the hands and forearms and is observed almost exclusively in persons who work intensively with fungi (fungus growers). Persons suffering from atopic eczema (neurodermatitis) may experience acute eczema flare-ups when exposed to fungal antigens, even if they do not have an actual allergy to fungi. Food allergies associated with eating edible mushrooms, e.g. porcini, shiitake or oyster mushrooms are rare, but they can occasionally be the cause of an alimentary allergy. The most common symptoms of mushroom allergy after consuming them are: generalised skin itching, abdominal pain and diarrhoea. More rarely, generalised hives (urticaria) or allergic shock (anaphylaxis) are observed.
HOW DO I FIND OUT IF I HAVE A FUNGAL ALLERGY?
Sensitisation to fungi can be detected by skin tests or measurements of specific IgE antibodies from the blood. However, the clinical significance is not always easy to assess, so additional tests are often needed. For eczema, patch or epicutaneous tests with fungal extracts can be performed.
WHAT CAN BE DONE ABOUT FUNGAL ALLERGY?
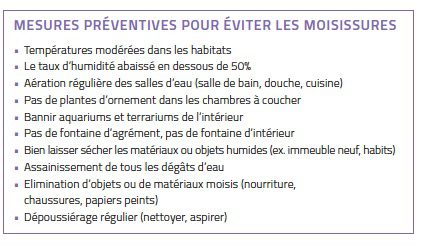
Since fungi occur everywhere, it is practically impossible to completely avoid contact with spores or fungal parts (e.g. mycelia). Nevertheless, measures can be taken in the home to make living conditions more difficult for fungal growth (see box). For the treatment of fungal allergies, the same medications are used as for “hay fever” or asthma. This usually alleviates the symptoms. Specific immunotherapies (hyposensitisation) with fungal extracts are rarely performed (e.g. with Alternaria or Cladosporium).
DISEASES ASSOCIATED WITH FUNGI:
– Allergic rhinitis, sinusitis and/or conjunctivitis
– Allergic fungal sinusitis and allergic bronchopulmonary mycosis
– Allergic asthma: exogenous allergic alveolitis
– Skin allergies (rarer): urticaria, atopic dermatitis, contact dermatitis.










0 Comments